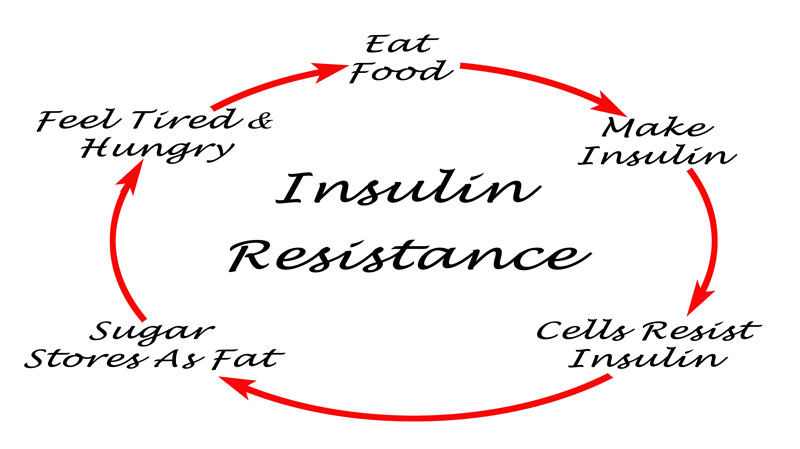
Insulin is a hormone made by the beta cells in the pancreas. When glucose levels rise after a meal, the pancreas releases insulin into the bloodstream to help the glucose enter into cells so it can be utilized for energy. With insulin resistance (IR), the pancreas has to work extra hard to keep up with the glucose demands (so insulin levels will rise). This process burns out the beta cells, rendering 80 - 90% of them ineffective by the time diabetes is diagnosed. IR typically leads to pre-diabetes (when glucose levels are higher than normal, but not high enough for the diagnosis of diabetes). Anyone who is pre-diabetic should be considered insulin resistant. Shockingly, 70% of people over the age of 30 are already IR, but these patients are rarely diagnosed or treated.
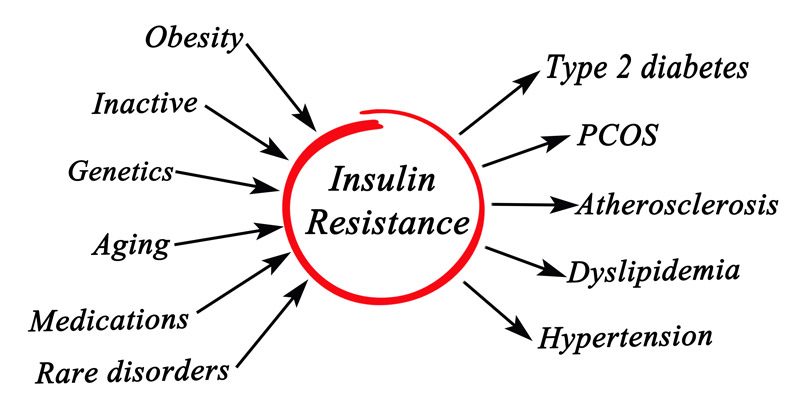
Though genetics play a small role, IR and pre-diabetes mostly develop from being overweight, smoking, physical inactivity, sleep apnea, and excessive dietary intake of carbohydrates (starchy/sugary foods). If caught early, lifestyle changes can be implemented (and sometimes medications prescribed) to preserve the beta cells in the pancreas and prevent the onset of diabetes.
IR/pre-diabetes typically occurs 5-15 years before the onset of diabetes but can cause many health problems before the full onset of diabetes. One of the nation’s leading endocrinologist in diabetes research, Dr. Ralph Defronzo, discovered that nearly 10% of pre-diabetics already have permanent microvascular damage, either neuropathy (nerve damage) or retinopathy (damage to the vessels behind the eyes), before they ever have diabetes! 1 In addition, IR and pre-diabetes typically cause vascular inflammation, which is the driving force behind many other detrimental diseases (heart disease, cancer, autoimmune disease, Alzheimer’s disease, etc.). By the time someone is diagnosed with diabetes, they typically already have atherosclerosis (plaque in the arteries that can lead to a heart attack or stroke). This is why early diagnosis and treatment of IR/pre-diabetes is so critical.
We run advanced blood panels on our patients to help identify those with insulin resistance, so we can address the disease before it causes detrimental (and possibly permanent) effects on the patient’s health. We run advanced blood panels on our patients to help identify those with insulin resistance, so we can address the disease before it causes detrimental (and possibly permanent) effects on the patient’s health.
How do you diagnose insulin resistance and pre-diabetes?
The most common blood sugar tests done at medical offices are fasting blood sugar and Ha1c (a three month average of blood sugars). If a patient’s fasting blood sugar is between 101-125, or their Ha1c is between 5.7 – 6.4, then they are considered pre-diabetic. However, even patients with a normal fasting blood sugar and Ha1c could still be insulin resistant.

Many patients are told their blood work is perfectly fine when in reality there are hidden metabolic risks they need to address. In a fasting state, the pancreas can often still produce enough insulin to keep the blood sugar normal. However, when there is a sudden surge in the blood sugar after eating or drinking carbohydrates, the fatigued beta cells in the pancreas have to work harder to crank out sufficient insulin to lower the blood sugars. As a result, insulin levels rise (so elevated insulin levels are an indication of insulin resistance, even before elevations in blood sugar). However, the 2hr oral glucose tolerance test (OGTT) test remains one of the best ways to assess one’s pancreatic function. You can read more about testing for IR and pre-diabetes HERE.
Historically the American Diabetes Association has defined an OGTT two-hour level of less than 140 mg/dL as “normal,” a level of 140-199 as pre-diabetes, and a level above 200 as diagnostic of diabetes. However, Dr. Ralph Defronzo, a world expert in diabetes, has published excellent data in peer-reviewed journals indicating that once the two-hour sugar reading reaches 120 mg/dL or higher, at least 60 percent of the beta cells are fatigued (also known as beta cell function loss). Once 90 percent are fatigued, the patient is a diabetic. Dr. Defronzo’s research demonstrated that if the one-hour sugar level goes above 125 mg/dL, or the two-hour level goes above 120, this person should be considered pre-diabetic. And if the one-hour goes above 150 mg/dL, or two-hour goes above 159, then this person is 13 times more likely than the average person to progress to diabetes in the next seven to eight years.
Can Pre-diabetes be reversed? How do you Treat Insulin Resistance?
Exercise is a key component to combating insulin resistance (IR) and reversing the disease process. Studies have shown that exercise helps the muscles become more sensitive to insulin - the more muscle mass someone has, the more glucose they can burn (which correlates to better blood sugar levels). 30 minutes or more of daily cardiovascular exercise (anything that gets your heart rate up and keeps it up) is ideal. When done daily, it can remove 88% of the inflammation in the vessels.

If exercise is not already a part of your normal regimen, it needs to be implemented. You can start with just 15 - 20 minutes a day of brisk walking and work up from there. (We can even do a CPET to determine your ideal heart rate zone for exercise, since this varies widely among individuals). If exercise is a physical challenge, we suggest finding a local pool, since water exercises are lower impact on the joints. Some patients who have pain with walking can tolerate exercise on a recumbent bike; others may do better using an upper body ergometer (a hand crank that looks like bicycle pedals for your hands). Affordable models can be purchased for in-home use.
Adopting healthy eating habits can certainly help reverse IR. Instead of trying extreme weight-loss solutions, people should slowly adopt healthy eating habits they can maintain. True success does not result from “going on a diet,” but rather long-term lifestyle changes for better health. The most important and effective dietary change for IR is decreasing overall carbohydrate intake. Carbohydrates are basically starches and sugars: bread, pasta, potatoes, rice, corn, and anything with sugar in it. Fruits have natural sugars so they need to be eaten in moderation (berries are best). Drinks with sugar (such as juice, sodas, and sweet tea) should be avoided. Natural sweeteners (Stevia, monk fruit, or sugar alcohols like erythritol and xylitol) are preferable because artificial sweeteners can raise insulin levels, and may even contribute to weight gain. 2 Read more about the ideal diet HERE.

Meals should consist mainly of meats and vegetables (and other low carbohydrate foods like eggs, nuts, healthy fats). It is best to eat keep carbohydrate intake as low as possible, at least under 25 grams per meal. Simply replacing one meal or snack a day with a healthy protein shake or protein bar can be a good first step. There are numerous resources to help educate patients on carbohydrate levels in different foods (Apps like My Fitness Pal or Lose It, or even just using Siri or Google).
Intermittent fasting (IF) is another effective way to improve IR and pre-diabetes. Dr. Jason Fung, leading expert on IF, has helped hundreds of patients reverse their diabetes (and even get off their insulin) through incorporating IF and a low carbohydrate diet. Losing just 5-10% of overall body weight can bring dramatic improvements in glucose and insulin levels.
Medication is sometimes prescribed to help treat the IR, preserve the beta cells in the pancreas, and delay or prevent the onset of diabetes. Ideally medications and lifestyle changes are paired together; this is the best possible combination to reverse IR and diabetes. Then in time, patients may be able to stop some of their medications if they maintain the appropriate lifestyle changes. Read more about natural supplements and prescription medications for pre-diabetes HERE.




