- Home
- About Us
- Advanced Testing
- Nutrition & Self-Care
- Further Learning
- New Member Info
- Contact
Apo B is a direct measurement of all the atherogenic particles that a patient has (VLDL, IDL, LDL, and Lipo (a)) so it is the most accurate measurement of "bad" cholesterol. On the other hand, LDL cholesterol is an indirect measurement based on a calculation, so lab results can vary up to 30% . . . and LDL cannot even be calculated if the patient’s triglycerides are too high.
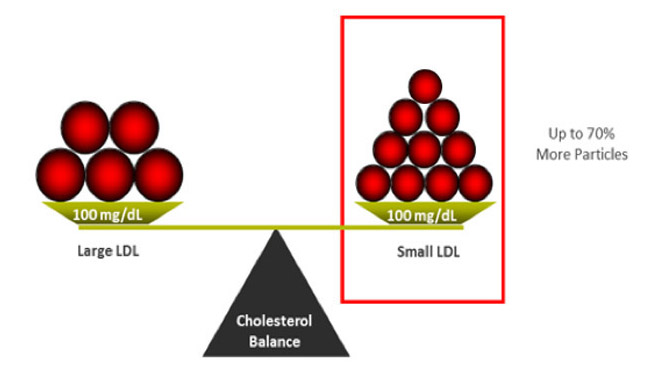
This slide is an example of two different patients who have the same LDL cholesterol (100 mg/dL), but their Apo B is different. Think of cholesterol like traffic in your arteries. You could have either 5 cars (cholesterol particles) with 20 cholesterol passengers (like on the left) or you could have 10 cars (cholesterol particles) with 10 cholesterol passengers (like on the right). Either way you are transporting 100 passengers (100 mg/dL of LDL cholesterol). The more cars (particles) you have, the more traffic in your arteries and the higher the CV risk. A higher Apo B level reveals this CV risk, as demonstrated in the patient on the right . . . which was not identified by the level of LDL cholesterol.
The ADA (American Diabetes Association), ACC (American College of Cardiology), and NLA (National Lipid Association) all endorse Apo B as superior to LDL-C for marking CV risk. There is no disputing the evidence.
In the Health Professionals Follow-Up Study, apo B was strongly associated with C-V risk, while LDL-C and non-HDL-C were NOT statistically significant. 11
In the AMORIS study, apo B was shown to be a significant predictor of fatal heart attack in both men and women, but LDL-C was insignificant in women (and only modestly associated in men). 10
In the EPIC study, LDL-C does not predict coronary artery disease (CAD) risk, but LDL particle number does (a surrogate marker of apo B). 1
In the JUPITER trial, baseline LDL-C was not associated with CV events, but apo B was. 2
In the CARDIA study, Apo B was determined to be a better predictor of coronary artery calcium score than LDL-C. 3
A large meta-analysis of twelve independent reports (including 233,455 subjects and 22,950 CV events) concluded that Apo B is the most potent marker of CV risk, LDL-C is the least, and non-HDL-C is intermediate. 7 Based on number of CVD events at 10 years, a treatment strategy that used Apo B instead of LDL-C would prevent 500,000 – 800,000 more CV events! 4 7
CONCLUSION: Apo B should be used to assess CV risk, not LDL-C.
Diet, exercise, and weight loss can all help lower Apo B. Interestingly, exercise has not been shown to decrease LDL-C much, but it does lower Apo B, so it is certainly still lowering the atherogenic burden and benefiting the patient. 25
Statin cholesterol medications are typically very effective at lowering Apo B levels. Sometimes niacin or zetia are added onto therapy to further lower levels. In the higher risk patient, PCSK9 inhibitors might be used - these are extremely effective at lowering Apo B levels.
Do something today for a better tomorrow!
Make an appointment now for advanced testing. We are here to help.
REFERENCES
1 – El Harchaoui, et. al. (2007). Value of Low-Density Lipoprotein Particle Number and Size as Predictors of Coronary Artery Disease in Apparently Healthy Men and Women: The EPIC-Norfolk Prospective Population Study. J Am Coll Cardiol, 49(5), 547-553.
2 – Mora, S., et. al. (2015). Atherogenic Lipoprotein Subfractions Determined by Ion Mobility and First Cardiovascular Events After Random Allocation to High-Intensity Statin or Placebo: The JUPITER Trial. Circulation. Doi:10.1161/circulationaha.115.016857
3 - Wilkins, J. T., et. al. (2016). Discordance Between Apolipoprotein B and LDL-Cholesterol in Young Adults Predicts Coronary Artery Calcification The CARDIA Study. J Am Coll Cardiol, 67(2), 193-201.
4 – Rosenson, R. S., Hegele, R. A., & Gotto, J. A. M. (2016). Integrated Measure for Atherogenic Lipoproteins in the Modern Era Risk Assessment Based on Apolipoprotein B. J Am Coll Cardiol, 67(2), 202 – 204.
5 – Circulation. 2000;101:477-484; Gotto, et. al.
6 – Lancet. 2003;361:777-780; Sniderman
7 - https://www.ncbi.nlm.nih.gov/pubmed/21487090
8 - https://www.aarp.org/health/healthy-living/info-2018/bob-harper-heart-attack-fd.html
9 – https://www.ncbi.nlm.nih.gov/pubmed/19081406
10 - https://www.ncbi.nlm.nih.gov/pubmed/11755609
11 - https://www.ncbi.nlm.nih.gov/pubmed/16316964
12 - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC80634/
13 - https://www.ahajournals.org/doi/10.1161/hc1002.105136
14 – Superko HR. Beyond LDL-C, Circ. 1996;94:2351-2354
15 – Akosah KO, Schaper A, Cogbill C. J Am Coll Cardiol. 2003;41(9):1475-1479.
16 – Berman et al. J Am Coll Cardiol. 2004;44:923-30.
17 – Grundy SM, et al. Circulation. 2005; 112:2735-2752
18 – Pearson TA et al, Circulation 2003;107:499-511
19 – Hlatky MA et al. Circulation 2009;119:2408-2416 3. Greenland P et al. Circulation 2007;115:402-426
20 – Greenland P et al. Circulation 2010;122:e584-e636
21 - https://www.healthline.com/health/heart-disease/statistics
22 - https://www.mayoclinicproceedings.org/article/S0025-6196(14)00800-3/pdf
23 - https://www.nejm.org/doi/full/10.1056/NEJMoa0807646
24 - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3165136/